
Your heart produces natriuretic peptides, powerful hormone-like substances that regulate your body’s fluid balance and blood pressure. These peptides counteract the effects of stress hormones that raise blood pressure, and their dysregulation can have significant implications for your cardiovascular health.
There are three main types of natriuretic peptides, each with unique structures and functions. They play an essential role in regulating blood pressure, electrolyte balance, and fluid homeostasis. As you explore the world of natriuretic peptides, you’ll discover how their functions impact your overall health and uncover the latest research on their therapeutic potential and clinical significance.
What Are Natriuretic Peptides?
Understanding natriuretic peptides begins with recognizing that they’re a group of hormone-like substances produced by your heart in response to changes in blood pressure.

Your heart produces these peptides to regulate fluid balance and blood pressure. By releasing them into your bloodstream, your heart sends signals to other parts of your body, such as your kidneys, to increase urine production and dilate blood vessels. This process reduces blood pressure and alleviates heart strain.
The biological significance of natriuretic peptides lies in their ability to counteract the effects of stress hormones that raise blood pressure.
Their clinical implications are substantial, as studies have shown that elevated levels can diagnose and monitor heart conditions like heart failure. Recognizing their functions can lead to a better understanding of cardiovascular health and disease prevention.
Types of Natriuretic Peptides
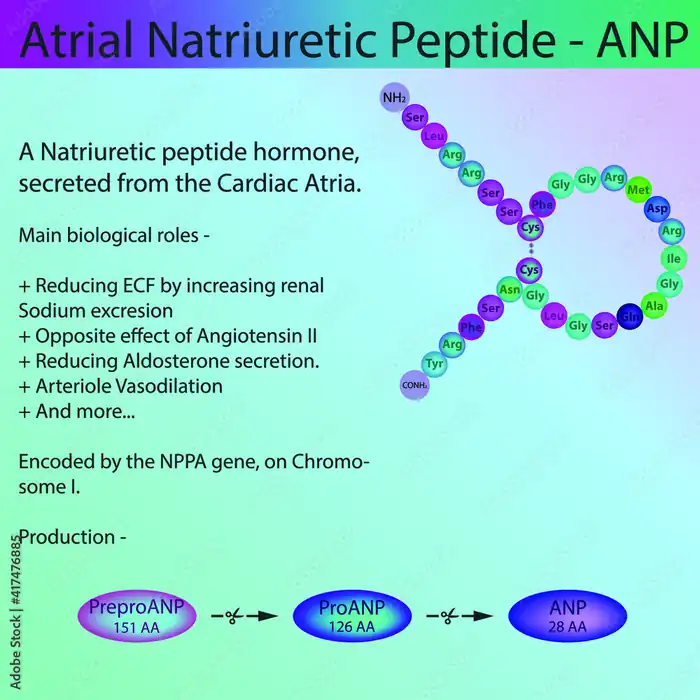
Natriuretic peptides come in several forms, including atrial natriuretic peptide (ANP), brain natriuretic peptide (BNP), and C-type natriuretic peptide (CNP), each of which plays a distinct role in the body.
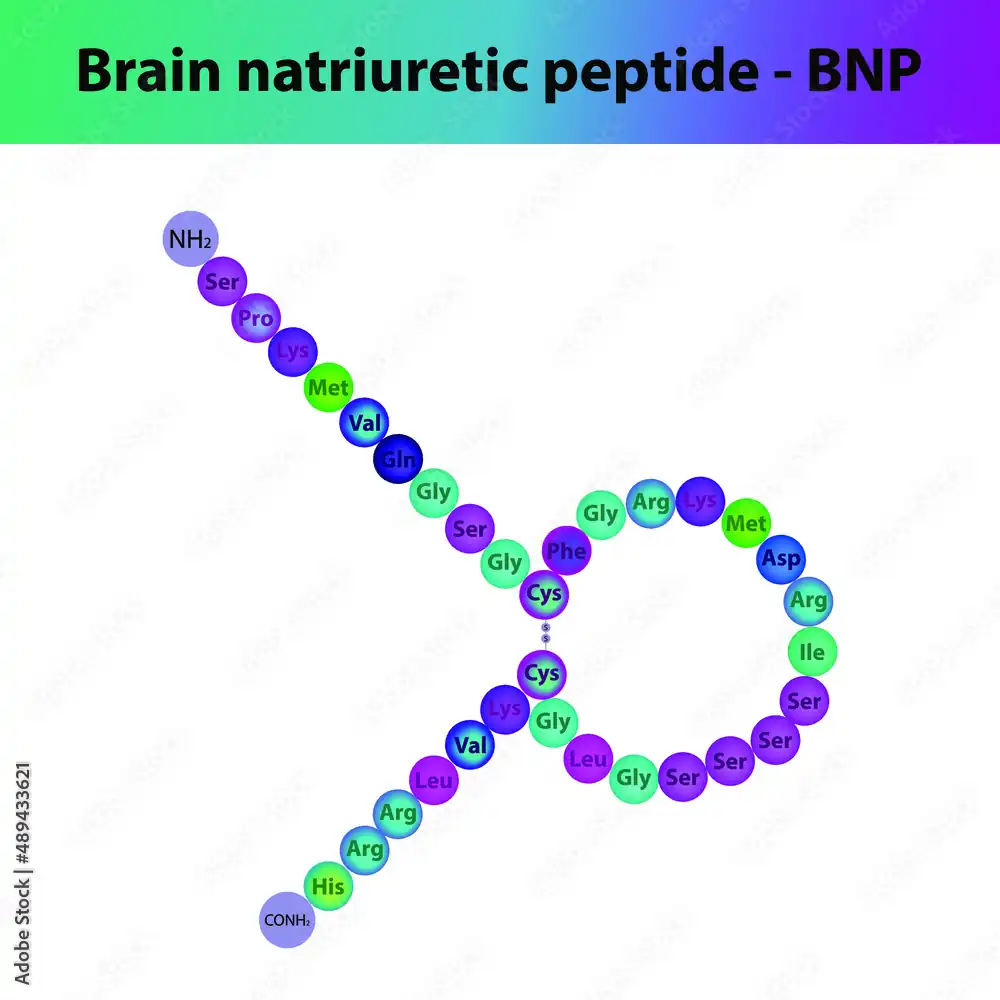
You’ll find ANP primarily in the heart’s atria, while BNP is concentrated in the ventricles. CNP, on the other hand, is found in the endothelial cells lining blood vessels.
The evolution of natriuretic peptides has led to their adaptation in various bodily functions. Their unique structures and functions make them useful in diagnostic applications, such as detecting heart failure and monitoring cardiovascular health.
By understanding the different forms of natriuretic peptides, you can better appreciate their importance in maintaining overall health and well-being.
Their distinct roles also open up possibilities for targeted treatments and therapies.
Functions and Roles
At the heart of cardiovascular health, atrial natriuretic peptides, brain natriuretic peptides, and C-type natriuretic peptides work together to orchestrate a delicate balance of bodily functions.
You’re probably wondering how they manage to do this. It all comes down to their unique functions and roles.
Here are the key functions of natriuretic peptides:
- Regulate blood pressure by promoting vasodilation and natriuresis
- Reduce cardiac hypertrophy and fibrosis
- Modulate the renin-angiotensin-aldosterone system
- Influence electrolyte balance and fluid homeostasis
- Play a role in cardiac remodeling and repair
Understanding the physiological significance of natriuretic peptides has major clinical implications.
It can help you diagnose and manage cardiovascular diseases, such as heart failure and hypertension, more effectively.
How Natriuretic Peptides Work
When your heart detects high blood pressure or stretching in its chambers, it releases natriuretic peptides, which then trigger a series of reactions to restore normal blood volume and pressure.
Your body synthesizes these peptides through a complex process involving natriuretic peptide synthesis, where precursor molecules are converted into the active peptides.
Once released, they interact with receptors in your blood vessels, kidneys, and adrenal glands, initiating a cascade of effects.
Through receptor interaction, natriuretic peptides stimulate the production of cyclic guanosine monophosphate (cGMP), an essential signaling molecule that relaxes blood vessels and promotes sodium and water excretion.
This intricate process allows your body to precisely control blood volume and pressure, ensuring ideal cardiovascular function.
Role in Blood Pressure Regulation
Natriuretic peptides help lower your blood pressure by promoting the excretion of sodium and water, reducing blood volume and easing the pressure on your blood vessels.
Lowering Blood Pressure
Natriuretic peptides play an essential role in lowering blood pressure by causing blood vessels to dilate, which reduces the pressure on vessel walls and decreases the heart’s workload.
Through complex natriuretic peptide mechanisms, these peptides modulate blood pressure by influencing various physiological processes. Here are some key ways they help lower blood pressure:
- Counteracting the effects of vasoconstrictors, such as angiotensin II and endothelin-1
- Relaxing vascular smooth muscle cells, leading to vasodilation
- Increasing sodium excretion, reducing fluid retention
- Antagonizing the sympathetic nervous system’s stimulation of the heart and blood vessels
- Reducing aldosterone levels, which decreases fluid retention and promotes vasodilation
Regulating Vascular Tone
Regulating vascular tone is a critical function of natriuretic peptides, which directly impact blood pressure by modulating the degree of blood vessel constriction or dilation.
As you explore the role of natriuretic peptides in blood pressure regulation, you’ll discover that they promote vascular health by enhancing endothelial function.
When your endothelial cells are functioning properly, they produce molecules that relax and dilate your blood vessels, reducing blood pressure.
Natriuretic peptides stimulate this process, allowing your blood vessels to respond more effectively to changes in blood flow.
As a result, your body can maintain healthy blood pressure levels, reducing the strain on your cardiovascular system.
Counteracting Vasoconstriction Effects
Your body also relies on natriuretic peptides to counteract the effects of vasoconstriction, a process that narrows your blood vessels and increases blood pressure.
Allowing these peptides to play a key role in maintaining the delicate balance of blood pressure regulation, they activate vasodilation mechanisms, causing your blood vessels to relax and widen, which in turn lowers blood pressure.
This is achieved through complex hormonal interactions involving various bodily systems.
Some key effects of natriuretic peptides on the cardiovascular system include:
- Inhibiting the release of vasoconstricting hormones
- Stimulating the release of vasodilating hormones
- Reducing blood vessel constriction
- Increasing blood vessel elasticity
- Enhancing sodium and water excretion to reduce blood volume
These actions combined help to counteract vasoconstriction effects, ensuring a healthy blood pressure balance.
Effect on Electrolyte Balance
By influencing the kidneys, these peptides play an essential role in maintaining electrolyte balance, particularly sodium and potassium levels, which in turn affects blood volume and pressure.
You see, natriuretic peptides help regulate electrolyte homeostasis by promoting the excretion of sodium and water.
This sodium regulation is critical, as it directly impacts blood pressure. When sodium levels increase, your blood vessels expand, and your blood pressure rises.
By stimulating sodium excretion, natriuretic peptides help reduce blood pressure and alleviate the strain on your cardiovascular system.
This delicate balance is fundamental for maintaining proper bodily functions, and natriuretic peptides are a key part of the process.
Impact on Fluid Volume
As natriuretic peptides work to maintain electrolyte balance, they also exert a significant influence on fluid volume, another critical factor in blood pressure regulation and overall cardiovascular health. You can think of them as your body’s fluid management specialists.
When fluid volume gets too high, they step in to reduce fluid retention and prevent volume overload. Here are some key ways they impact fluid volume:
- Increase urine production to eliminate excess fluids
- Reduce fluid absorption in the kidneys
- Counteract the effects of volume-expanding hormones like aldosterone
- Lower blood pressure by reducing vascular resistance
- Help your body get rid of excess salt and water through the kidneys and urine
Relationship With Heart Failure
You can effectively use B-type natriuretic peptide (BNP) levels to gauge the severity of heart failure, and monitoring these levels can help you manage the condition more effectively.
Diagnosing Heart Failure Risk
Your doctor may use natriuretic peptides to gauge your risk of heart failure, as elevated levels of these biomarkers are frequently associated with increased risk.
During patient assessment, they’ll consider your medical history, physical exam results, and heart failure symptoms, such as shortness of breath, fatigue, and swelling.
Some factors that may indicate a higher risk of heart failure include:
- Elevated levels of natriuretic peptides, such as BNP or NT-proBNP
- Abnormal electrocardiogram (ECG) or echocardiogram results
- History of heart disease, high blood pressure, or diabetes
- Family history of heart failure
- Presence of other medical conditions, such as kidney disease or sleep apnea
Managing BNP Levels Effectively
Effective management of BNP levels is essential in reducing the risk of heart failure, and it typically involves a combination of lifestyle modifications, medication, and regular monitoring.
When your BNP levels are high, you’ll need to work closely with your doctor to develop a personalized plan to lower them.
BNP management strategies may include lifestyle modifications such as reducing sodium intake, exercising regularly, and managing stress.
You’ll also need to monitor your condition regularly, tracking changes in your symptoms and BNP levels.
By taking these proactive steps, you can considerably reduce your risk of heart failure and stay on top of your condition.
Connection to Kidney Function
Because the kidneys play an essential role in regulating fluid balance and blood pressure, natriuretic peptides have a significant connection to kidney function.
You’ll notice that when your kidneys aren’t working well, your natriuretic peptide levels are affected. Here are some key points to take into account:
- Your kidneys produce natriuretic peptides to help regulate fluid balance and blood pressure.
- Natriuretic peptides help reduce fluid retention, which can put a strain on your kidneys.
- Kidney health is closely linked to natriuretic peptide function.
- Changes in natriuretic peptide levels can indicate kidney problems.
- Maintaining healthy blood pressure and preventing fluid retention are vital for supporting kidney health.
Natriuretic Peptide Testing
Natriuretic peptide testing helps diagnose and monitor conditions related to heart and kidney function by measuring the levels of these peptides in your blood.
You’ll undergo this test if you’re experiencing symptoms like swelling, shortness of breath, or chest pain, which could indicate heart failure or kidney disease.
The test provides essential information about your condition’s severity and helps your doctor determine the best course of treatment.
Natriuretic peptide applications include monitoring the effectiveness of treatment and detecting potential complications.
By following natriuretic peptide guidelines, your healthcare provider can guarantee accurate test results and make informed decisions about your care.
Regular testing helps track changes in your peptide levels, enabling adjustments to your treatment plan as needed.
This guarantees you receive the most effective care for your condition.
Clinical Significance and Diagnosis
How do elevated levels of natriuretic peptides in your blood influence the diagnosis and management of conditions like heart failure and kidney disease?
These peptides serve as diagnostic markers, helping your doctor diagnose and monitor these conditions. Elevated levels can indicate heart failure, kidney disease, or other cardiovascular conditions.
Here are some key points about the clinical significance and diagnosis of natriuretic peptides:
- Elevated levels can indicate left ventricular dysfunction or heart failure.
- Natriuretic peptides can help diagnose acute kidney injury.
- They can also help monitor the effectiveness of treatment for heart failure and kidney disease.
- Abnormal levels can indicate an increased risk of cardiovascular events.
- Natriuretic peptides have clinical applications in diagnosing and managing conditions such as hypertension, pulmonary embolism, and acute coronary syndrome.
FAQs
1. What are natriuretic peptides?
Natriuretic peptides are a family of hormones primarily involved in the regulation of blood pressure, blood volume, and sodium balance. They exert their effects through specific natriuretic peptide receptors.
2. What is the natriuretic peptide system?
The natriuretic peptide system is a complex network of peptides, including atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP), that work together to maintain cardiovascular homeostasis. It plays a critical role in heart function and blood pressure regulation.
3. Who produces natriuretic peptides?
Natriuretic peptides are produced by the heart and other organs. For example, ANP is primarily secreted by the cardiac atria, while BNP is produced in both the ventricles and the brain (originally called brain natriuretic peptide).
4. What are natriuretic peptide receptors?
Natriuretic peptide receptors are specialized proteins that bind natriuretic peptides to mediate their biological effects. Known receptors include natriuretic peptide receptor-a, natriuretic peptide receptor-b, and natriuretic peptide receptor-c.
5. How are natriuretic peptides useful in treating heart failure?
Natriuretic peptides help in the management of heart failure by promoting vasodilation, natriuresis, and diuresis. They are particularly beneficial for patients with heart failure, both acute and chronic.
6. What is the role of natriuretic peptide concentrations in diagnosis?
Plasma natriuretic peptide levels, including BNP and n-terminal pro-brain natriuretic peptide, are commonly used biomarkers in the diagnosis of heart failure. Elevated natriuretic peptide concentrations indicate heart stress and can be used to assess the severity.
7. How effective are natriuretic peptides in treating acutely decompensated heart failure?
Options like nesiritide, a recombinant form of BNP, have been used in the treatment of acutely decompensated heart failure due to their potent vasodilating properties.
8. Can natriuretic peptides be used in patients with chronic heart failure?
Yes, monitoring natriuretic peptide levels, such as BNP and ANP, can be valuable in the ongoing management of chronic heart failure. These peptides help in assessing the progression and treatment efficacy in chronic heart failure patients.
9. What is the link between natriuretic peptides and renal function?
Natriuretic peptides promote renal natriuresis and diuresis. However, in patients with acute renal failure or chronic kidney disease, the levels of natriuretic peptides can be elevated, complicating their diagnostic utility.
10. Are there any genetic factors involved in natriuretic peptide function?
The human natriuretic peptide receptor gene and its variants can affect the receptor status and the overall effectiveness of natriuretic peptide signaling.